Bursitis Of The Foot Treatment Method
Retrocalcaneal bursitis is an inflammation or infection of the bursae at the back of the heel bone. Bursae are fluid-filled sacs that cushion the joints and prevent the bones from becoming injured due to friction. Because this condition can cause pain and difficulty moving, getting treatment is important. There are several retrocalcaneal bursitis treatment options available. Patients and physicians should work together to determine the best treatment based on the symptoms and severity of the condition.
Causes
Systemic diseases such as rheumatoid arthritis, ankylosing spondylitis, reactive arthritis, psoriatic arthritis, scleroderma, systemic lupus erythematosus, pancreatitis, Whipple disease, oxalosis, uremia, hypertrophic pulmonary osteoarthropathy, and idiopathic hypereosinophilic syndrome have also been associated with bursitis.
Symptoms
Medical experts strongly recommend that you consult a doctor if you have any of the symptoms below. Disabling joint pain that prevents you from doing your daily activities. Pain that lasts for more than two weeks. Excessive swelling, redness, bruising or a rash around the painful joint. Sharp or shooting pain, especially when you exercise or do something more strenuous. A fever. Any of the above could be a sign of infection, a condition such as arthritis or a more serious injury such as a tendon tear that may require medical attention.
Diagnosis
During the physical examination of a patient with calcaneal bursitis, the physician should keep the following considerations in mind. Swelling and redness of the posterior heel (the pump bump) may be clearly apparent. The inflamed area, which may be slightly warm to the touch, is generally tender to palpation. Careful examination can help the clinician to distinguish whether the inflammation is posterior to the Achilles tendon (within the subcutaneous calcaneal bursa) or anterior to the tendon (within the subtendinous calcaneal bursa). Differentiating Achilles tendinitis/tendinosis from bursitis may be impossible. At times, the 2 conditions co-exist. Isolated subtendinous calcaneal bursitis is characterized by tenderness that is best isolated by palpating just anterior to the medial and lateral edges of the distal Achilles tendon. Conversely, insertional Achilles tendinitis is notable for tenderness that is located slightly more distally, where the Achilles tendon inserts on the posterior calcaneus. A patient with plantar fasciitis has tenderness along the posterior aspect of the sole, but he/she should not have tenderness with palpation of the posterior heel or ankle. A patient with a complete avulsion or rupture of the Achilles tendon demonstrates a palpable defect in the tendon, weakness in plantarflexion, and a positive Thompson test on physical examination. During the Thompson test, the examiner squeezes the calf. The test is negative if this maneuver results in passive plantarflexion of the ankle, which would indicate that the Achilles tendon is at least partially intact.
Non Surgical Treatment
Many times, Achilles tendon bursitis can be treated with home care. However, if self-care remedies do not work, your doctor may need to administer additional treatments. Home care. The most important thing you can do to help your healing is to refrain from activities that could further aggravate the bursitis. Typical home-care treatments for Achilles tendon bursitis include Anti-inflammatory medication. Take over-the-counter pain medication, like aspirin or ibuprofen, to reduce pain and swelling. Heel wedges. An over-the-counter or custom heel wedge can be placed in your shoe to minimize stress in the Achilles tendon. Ice. Apply ice or other cold therapy to your sore heel several times a day. Rest. Limit your activity on the injured leg, avoid putting pressure on it whenever possible. Also, elevate your leg during non-use to help reduce the swelling. The above remedies may be used on their own or in combination with others on the list. Physician-administered treatments. If the above self-care remedies are not effective, you should visit your doctor for additional treatment. Possible Achilles tendon bursitis treatments your doctor may administer include immobilization. If the bursitis is combined with Achilles tendonitis, your doctor may place a temporary cast on the ankle to prevent movement and allow it to heal. Physical therapy. Exercises may be used to improve the ankle's strength and flexibility. Steroids. Injection of steroids into the retrocalcaneal bursa (not the Achilles tendon) may be necessary. Surgery. In very rare circumstances, surgery may be needed to remove the retrocalcaneal bursa, however, this is typically a last resort.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
Prevention
Maintain proper form when exercising, good flexibility, and strength around the ankle to help prevent this condition from arising. Proper stretching of the achilles tendon helps prevent injury.
Hammer Toe Inducing Ball Of Foot Pain
 Overview
Overview
Hammer toes, Claw and Mallet Toe are similar conditions, all caused by deformity of the toe joints. They usually develop slowly from wearing poor fitting shoes, but can also be due to muscle or nerve damage. Muscle imbalance causes the toes to bend into odd positions which can be extremely painful, limiting walking and activity. They become more common with aging and affect approximately 10-15% of the population. Women are five times more likely to suffer from hammer, claw or mallet toe than men.
Causes
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A mallet toe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the mallet toe against the top of the shoe can lead to pain and the development of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort. Arthritis can also lead to many forefoot deformities including mallet toes. Mallet toes can cause extreme discomfort, and can be aggravated if restrictive or improperly fitting footwear is worn for a prolonged period of time.
 Symptoms
Symptoms
A hammertoe may be present but not always painful unless irritated by shoes. One may have enlarged toe joints with some thickened skin and no redness or swelling. However, if shoes create pressure on the joint, the pain will usually range from pinching and squeezing to sharp and burning. In long standing conditions, the dislocated joints can cause the pain of arthritis.
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Non Surgical Treatment
Putting padding between your toes and strapping them in place can help to stop pain caused by the toes rubbing. Custom-made insoles for your shoes will help to take the pressure off any painful areas. Special shoes that are wider and deeper than normal can stop your toes rubbing. However if your pain persists your consultant may recommend an surgery.
Surgical Treatment
There are several surgical techniques used to treat hammertoes. When the problem is less severe, the doctor will remove a small piece of bone at the involved joint and realign the toe joint. More severe hammer toes may need more Hammer toe complicated surgery.
 Prevention
Prevention
Preventing foot problems, including hammertoes, is often a matter of wearing the right shoes and taking care of your feet. Check your feet regularly for problems. This is especially true if you have diabetes or any other medical condition that causes poor circulation or numbness in your toes. If you do, check feet daily so that problems can be caught early on.
What Are The Treatments For Bunions?
Overview
 Bunions (hallux valgus) are often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. With a bunion, the big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment, producing the bunion's "bump." Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which continues to become increasingly prominent. Bunions can be painful, but not always. Bunions are always progressive, so the deformity becomes more prounced over time, even if its not painful.
Bunions (hallux valgus) are often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. With a bunion, the big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment, producing the bunion's "bump." Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which continues to become increasingly prominent. Bunions can be painful, but not always. Bunions are always progressive, so the deformity becomes more prounced over time, even if its not painful.
Causes
The exact cause of bunions is unknown, but they tend to run in families. Wearing badly fitting shoes is thought to make bunions worse. It's also thought that bunions are more likely to occur in people with unusually flexible joints, which is why bunions sometimes occur in children. In some cases, certain health conditions, such as rheumatoid arthritis and gout, may also be responsible.
Symptoms
The initial symptom may be pain at the joint prominence when wearing certain shoes. The joint capsule may be tender at any stage. Later symptoms may include a painful, warm, red, cystic, movable, fluctuant swelling located medially (adventitial bursitis) and swellings and mild inflammation affecting the entire joint (osteoarthritic synovitis), which is more circumferential. With hallux limitus or rigidus, there is restriction of passive joint motion, tenderness at the dorsolateral aspect of the joint, and increased dorsiflexion of the distal phalanx.
Diagnosis
Before examining your foot, the doctor will ask you about the types of shoes you wear and how often you wear them. He or she also will ask if anyone else in your family has had bunions or if you have had any previous injury to the foot. In most cases, your doctor can diagnose a bunion just by examining your foot. During this exam, you will be asked to move your big toe up and down to see if you can move it as much as you should be able to. The doctor also will look for signs of redness and swelling and ask if the area is painful. Your doctor may want to order X-rays of the foot to check for other causes of pain, to determine whether there is significant arthritis and to see if the bones are aligned properly.
Non Surgical Treatment
When the deformity is mild, treatment is usually not necessary. However, changing shoes to ones that have little or no heel, and are wider in the toe area (toe box) will be more comfortable and may help to prevent worsening of the bunion deformity. If the bunion starts to become painful, other measures may help. Bunions can cause pain in several different areas. The medial eminence may be painful, the entire first toe joint may hurt, or there may be pain underneath some or all of the forefoot (the ball of the foot). Pain over the medial eminence is the most common problem that affects bunion patients. A ?toe spacer? can be placed between the first and second toes and can provide some pain relief as it straightens out the bunion slightly. Pads placed over the medial eminence itself are hard to keep in place and rarely help to relieve pain. Pain underneath the first toe or lesser toes can be relieved by pads placed in the shoes in precise areas. The pads help to take pressure off the prominent areas on the bottom of the foot. Generalized measures to relieve bunion pain, such as physical therapy or foot stretching exercises, have not been shown to be helpful. Orthotics are often prescribed, but are also rarely helpful in relieving pain over the bunion, but may help with pain felt under the ball of the foot.
Surgical Treatment
The type of surgical procedure performed depends upon the severity of the bunion, the individual?s age, general health, activity level, and the condition of the bones and connective tissue. Other factors may influence the choice of a procedure used. Mild bunion. For this type of surgery, the surgeon may remove the enlarged portion of bone and realign the muscles, tendons, and ligaments surrounding the joint. Moderate bunion. For a moderate bunion, the surgeon may cut the bone and shift it to its proper position. Whether or not the bone is cut depends on the severity and location of the deformity. In addition, the surrounding tendons and ligaments may need to be repositioned. Severe bunion. For a severe bunion, surgery may involve removing the enlarged portion of the bone, cutting and realigning the bone, and correcting the position of the tendons and ligaments. Arthritic bunion or big toe joint. If the joint is damaged beyond repair, as is commonly seen in arthritis, it may need to be reconstructed or replaced with an artificial joint. Joint replacement implants may be used in the reconstruction of the big toe joint.
Overpronation Of The Feet
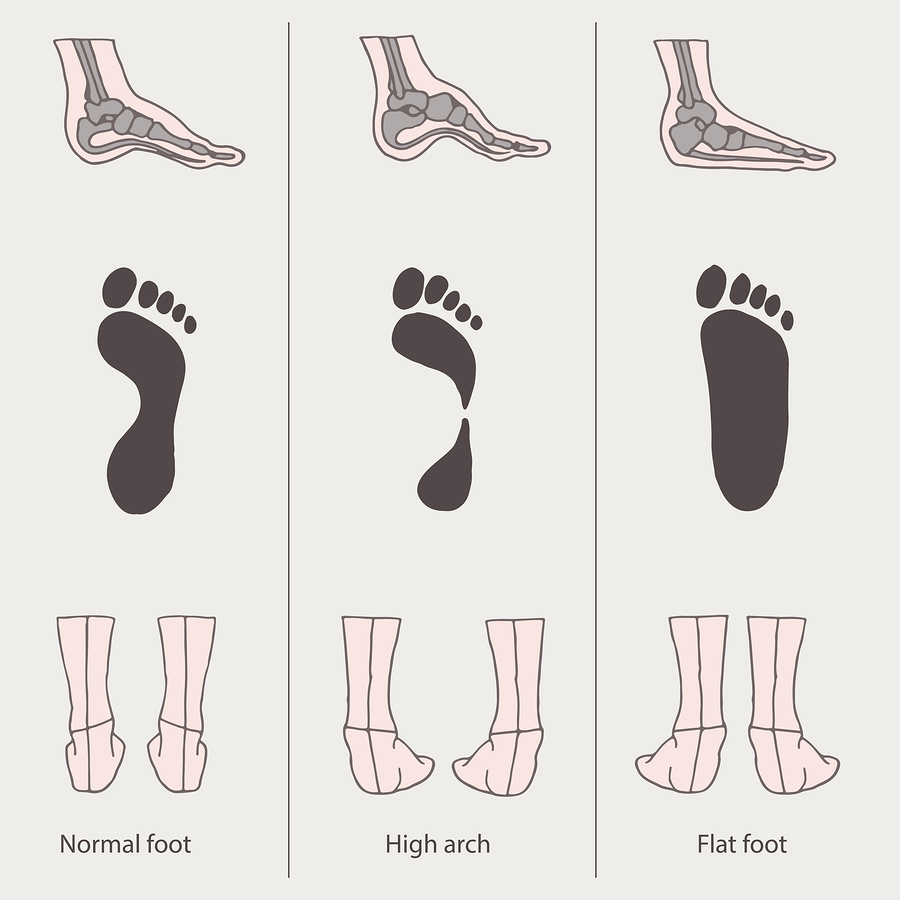
The anatomy of a normal foot allows for both to occur at the same time. Approximately 30% of the population have a normal foot. The remainder of people either overpronate (95% of abnormal feet) or oversupinate (5% of abnormal feet). The important thing to know is that all feet pronate and supinate, but abnormal feet do one of these things too much or at the wrong time. When the foot overpronates or oversupinates, several foot ailments can develop.
Causes
Abnormal foot biomechanics usually causes over-use type injuries, occurring most frequently in runners. When a neutral foot pronates during walking or running, the lower leg, knee and thigh all rotate internally (medially). When an athlete with an overpronated foot runs, this rotation movement is exaggerated and becomes more marked.
Symptoms
Symptoms can manifest in many different ways. Here is a list of some of the common conditions associated with over-pronation in children. Achilles Pain. Ankle pain. Arch Pain. Low back pain. Heel Pain. Knee Pain (Runner's knee and Chondromalecia of the patella) Osgood Schlatter Disease (pain below the knee) Shin Splints (pain in the front of the lower leg) Over-pronation does not necessarily mean your child has "flat feet." Even though children's arches may be relatively high when they lie down or sit, over-pronation may not be seen until your child is standing. A certain amount of pronation is normal. During normal walking or running ("gait cycle"), the heel strikes the ground and the foot rolls inward to absorb shock and adapt to the surface. This gait cycle is even more important if the running surface is uneven.
Diagnosis
To easily get an idea of whether a person overpronates, look at the position and condition of certain structures in the feet and ankles when he/she stands still. When performing weight-bearing activities like walking or running, muscles and other soft tissue structures work to control gravity's effect and ground reaction forces to the joints. If the muscles of the leg, pelvis, and feet are working correctly, then the joints in these areas such as the knees, hips, and ankles will experience less stress. However, if the muscles and other soft tissues are not working efficiently, then structural changes and clues in the feet are visible and indicate habitual overpronation.

Non Surgical Treatment
An orthotic is a device inserted inside the shoe to assist in prevention and/or rehabilitation of injury. Orthotics support the arch, prevent or correct functional deformities, and improve biomechanics. Prescription foot orthoses are foot orthoses which are fabricated utilizing a three dimensional representation of the plantar foot and are specifically constructed for an individual using both weightbearing and nonweightbearing measurement parameters and using the observation of the foot and lower extremity functioning during weightbearing activities. Non-prescription foot orthoses are foot which are fabricated in average sizes and shapes in an attempt to match the most prevalent sizes and shapes of feet within the population without utilizing a three dimensional representation of the plantar foot of the individual receiving the orthosis.
Prevention
Custom-made orthotics supports not only the arch as a whole, but also each individual bone and joint that forms the arch. It is not enough to use an over-the-counter arch support, as these generic devices will not provide the proper support to each specific structure of the arch and foot. Each pronated foot?s arch collapses differently and to different degrees. The only way to provide the support that you may need is with a custom-made device. This action of the custom-made orthotic will help to prevent heel spurs, plantar fasciitis, calluses, arch pain, and weakness of the entire foot.
What Exactly Is Calcaneal Apophysitis?
Pain in the heel of a child's foot, typically brought on by some form of injury or trauma, is sometimes Sever's Disease. The disease often mimics Achilles tendonitis, an inflammation of the tendon attached to the back of the heel. A tight Achilles tendon may contribute to Sever's Disease by pulling excessively on the growth plate of the heel bone. This condition is most common in younger children and is frequently seen in the active soccer, football or baseball player. Sport shoes with cleats are also known to aggravate the condition. Treatment includes calf muscle stretching exercises, heel cushions in the shoes, and/or anti-inflammatory medications. Consult your physician before taking any medications.
Causes
Young athletes typically sustain the injury due to repeated stress caused by running and jumping. Partaking in any high speed sports can thus partly provoke the condition, such as football, rugby, basketball, hockey or track athletics. Crucially the injury is linked to overuse, so exercising with fatigued leg muscles, without a suitable warm up, or beginning a new strenuous physical activity are all risk factors. Placing excessive weight or pressure on the heel can also cause the injury. Another factor related to Sever's disease is overpronation, a biomechanical error that makes the foot roll too far inwards.
Symptoms
This is a condition that affects the cartilage growth plate and the separate island of growing bone on the back of the heel bone. This growth plate is called the physeal plate. The island of growing bone is called the apophysis. It has the insertion attachment of the Achilles tendon, and the attachment of the plantar fascia. This island of bone is under traction from both of these soft tissue tendon and tendon-like attachments.
Diagnosis
Sever?s disease can be diagnosed based on the symptoms your child has. Your child?s doctor will conduct a physical examination by squeezing different parts of your child?s foot to see if they cause any pain. An X-ray may be used to rule out other problems, such as a broken bone or fracture.
Non Surgical Treatment
When the condition flares, it is treated with activity limitation, medication to reduce inflammation (such as ibuprofen [Advil] or naproxen [Aleve]), shoe inserts, heel lifts, cold packs, and sometimes casting when it becomes especially severe. Sever condition is generally a self-limited problem that usually improves within a year.
Recovery
Sever?s disease is self-recovering, meaning that it will go away on its own when the foot is used less or when the bone is through growing. The condition is not expected to create any long-term disability, and expected to subside in 2-8 weeks. The disease may also take several years to stop, because it is often triggered by growing too fast. It is more common in boys, although occurs in girls as well. The average age of symptom onset is 9-11.
Working With An Achilles Tendon Rupture
Overview
 The Achilles tendon is the largest and strongest tendon in the human body. The Achilles tendon connects the heel bone (calcaneus) to the muscles at the back of the calf (using gastrocnemius and soleus muscles). The synchronous function of the tendon and calf muscles is critical for activities like jumping, running, standing on the toe, and climbing stairs. When climbing stairs or running, the forces within the tendon have been measured and indicate that the structure is able to withstand at least 10 times the body weight of the individual. The function of the Achilles tendon is to help raise your heel as you walk. The tendon also assists in pushing up the toes and lifting the rear of the heel. Without an intact Achilles tendon, almost any motion with the ankle (for example, walking or running) is difficult.
The Achilles tendon is the largest and strongest tendon in the human body. The Achilles tendon connects the heel bone (calcaneus) to the muscles at the back of the calf (using gastrocnemius and soleus muscles). The synchronous function of the tendon and calf muscles is critical for activities like jumping, running, standing on the toe, and climbing stairs. When climbing stairs or running, the forces within the tendon have been measured and indicate that the structure is able to withstand at least 10 times the body weight of the individual. The function of the Achilles tendon is to help raise your heel as you walk. The tendon also assists in pushing up the toes and lifting the rear of the heel. Without an intact Achilles tendon, almost any motion with the ankle (for example, walking or running) is difficult.
Causes
The causes of an Achilles tendon rupture are very similar to Achilles tendinitis. Causes include. Running uphill. Running on a hard surface. Quickly changing speeds from walking to running. Playing sports that cause you to quickly start and stop.
Symptoms
When the Achilles tendon ruptures a loud bang or popping sound may be heard. The person may feel that they have been hit or kicked in the back of the lower leg and often they will look over their shoulder to see who or what has hit them. This is quickly followed by the sudden onset of sharp pain in the tendon and a loss of strength and function. If a complete rupture has occurred it may not be possible to lift the heel off the ground or point the toes. Often the degree of pain experienced, or lack of it, can be inversely proportional to the extent of the injury, ie a partial rupture may in fact be more painful than a complete rupture.
Diagnosis
In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests.
Non Surgical Treatment
Non-surgical treatment of Achilles tendon rupture is usually reserved for patients who are relatively sedentary or may be at higher risk for complications with surgical intervention (due to other associated medical problems). This involves a period of immobilization, followed by range of motion and strengthening exercises; unfortunately, it is associated with a higher risk of re-rupture of the tendon, and possibly a less optimal functional outcome. 
Surgical Treatment
The surgical repair of an acute or chronic rupture of the Achilles tendon typically occurs in an outpatient setting. This means the patient has surgery and goes home the same day. Numbing medicine is often placed into the leg around the nerves to help decrease pain after surgery. This is called a nerve block. Patients are then put to sleep and placed in a position that allows the surgeon access to the ruptured tendon. Repair of an acute rupture often takes somewhere between 30 minutes and one hour. Repair of a chronic rupture can take longer depending on the steps needed to fix the tendon.
Prevention
Here are some suggestions to help to prevent this injury. Corticosteroid medication such as prednisolone, should be used carefully and the dose should be reduced if possible. But note that there are many conditions where corticosteroid medication is important or lifesaving. Quinolone antibiotics should be used carefully in people aged over 60 or who are taking steroids.